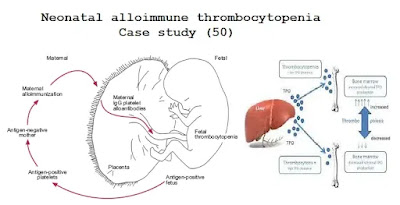
Case study (50) – Neonatal alloimmune thrombocytopenia
A full-term newborn was found to have purpura, petechiae, and
breathing difficulties.
A full blood count show:
Hemoglobin (Hb) 173 g/L
White blood cells (WBC) 16.4 × 109/L
Platelets 4 × 109/L
A computed tomography (CT) scan was performed. The mother had a pregnancy experience 4 years ago, and there were no complications in this pregnancy.
Questions:
Q1. Comment on the appearance of the CT scan.
Q2. What important causes would you consider for thrombocytopenia?
Q3. How should the child be treated?
Q4. What advice would you give regarding future pregnancy?
Answers:
A1. The CT scan shows evidence of acute
hemorrhage.
A2. Important causes of neonatal
thrombocytopenia are genetic, congenital, and acquired.
Genetic causes are rare but include thrombocytopenia with absent radii
(TAR) syndrome.
Congenital infections (rubella, cytomegalovirus [CMV], and
toxoplasmosis) should be ruled out through maternal serological testing and
neonatal culture studies.
Congenital immune thrombocytopenia may arise through the transplacental
passage of IgG antiplatelet antibodies in mothers with idiopathic thrombocytopenic
purpura or may present as neonatal alloimmune thrombocytopenia. Mothers who
lack certain platelet antigens (most commonly human platelet antigen [HPA]-1a)
will make antibodies if sensitized by previous pregnancy or transfusion.
Acquired causes include disseminated intravascular coagulation, sepsis,
and drugs.
A3. Maternal serum was found to contain anti-HPA-1A antibodies.
The mother’s platelets were HPA-1A negative, and the father and
both children were HPA-1A positive (as are more than 95% of people).
Therefore, the diagnosis was neonatal alloimmune thrombocytopenia.
The child received a transfusion of HPA-1A-negative platelets,
which were continued until the child was able to maintain an unsupported count
of more than 50 ×
109/L.
This occurred within 3 weeks as the titer of transplacentally
derived antibody fell.
High-dose intravenous immunoglobulin may also help increase
neonatal platelet counts.
A4. The partner should be tested and, if he is homozygous HPA-1a
positive, as is likely, then future children will be affected.
The fetal platelet count can be monitored during pregnancy, if
necessary, HPA-1a negative platelets can be transfused as prophylaxis against
bleeding. Delivery should be performed by elective cesarean section.
All blood components for intrauterine transfusion should be CMV
negative and irradiated to minimize the risk of graft versus host disease.


Comments
Post a Comment