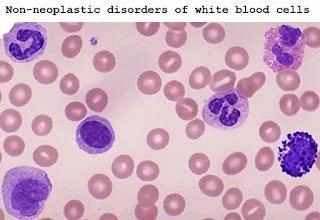
Non-neoplastic disorders of white blood cells
Disorders of white cells include deficiencies and proliferation, and they may be reactive or neoplastic
- Quantitative: Change in number
- Increase in number = Cytosis / philia
- Decrease in number = Cytopenia
- Qualitative: •Morphologic changes
•Functional changes
Quantitative changes:
- Relative vs Absolute values
• Total white blood cell count
• Differential count
• Absolute count
- Differentials offer the relative percentage of each white blood cell
- Absolute value offer the actual number of each WBC/mm3 of blood:
Calculation: absolute count= Total WBC x percent
- Regulation of cell production
• The regulatory mechanism must operate in a strictly controlled manner.
- Hemopoietic growth factors
- The control of cell death
- Inhibitors of cell proliferation
- Stromal cell factors (cell-cell and cell-matrix interaction).
Leucocytes
- Phagocytes:
• Granulocytes: Neutrophils, Eosinophils, Basophils
• Mononuclear phagocytes: monocytes, macrophages, and dendritic cells
• Lymphocytes: B-cells, T-cells
Quantitative changes (LEUCOCYTOSIS)
- An increase in TWBC caused by an increase in any of a single bloodline.
- Note: The increase in the minor cell population can occur without an increase in the total white blood cell count.
- Normal reference range (adult 21 years): 4.5 -11.0 x 109/L.
Quantitative changes (LEUCOPENIA)
- TWBC below the age reference range is defined as leukopenia
- Leukopenia may affect one or more lineages and may have severe neutropenia or lymphopenia without a decrease in the total number of white blood cells.
Granulocytosis
- Increased counts of all or one granulocyte component: neutrophils, basophils, eosinophils
- Agranulocytosis: reduction of all or one granulocyte component
Quantitative changes (NEUTROPHILIA)
- Increased number of neutrophils and/or their precursors
- Count in adults >7.5 x 109/L but the counts dependent on age.
- The increase may be due to the following normal steady-state changes:
1. Production:
- Increased progenitor cell proliferation
- Increased frequency of committed neutrophil precursor cell division
2. Transit: Impaired transit to tissue
3. Migration
4. Destruction
Causes of Neutrophilia
1. Bacterial Infection
2. Inflammatory conditions: Autoimmune disorders, Gout
3. Neoplasia
4. Metabolic conditions: Uremia, Acidosis, Hemorrhage
5. Corticosteroids
6. Marrow infiltration/fibrosis
7. Myeloproliferative disorders
Acute Neutrophilia
a. The adrenaline stress test shows that it can be quickly mobilized under pressure, due to the decreased adhesion of neutrophils:
1. Bacterial infection
2. Stress
3. Exercise
b. Slower rise when cells are released from the bone marrow storage pool:
1. Steroid
2. Infections such as (reactive changes; left shift, toxic granulation, high NAP score, and Dohle bodies.
c. Steroids also reduces the passage to the tissues
Chronic neutrophilia
- Long term corticosteroid therapy
- Chronic inflammatory reactions
- Infections or chronic blood loss
- Infections: Less common organisms e.g., poliomyelitis
• Leukemoid reactions
- Suitable for chronic neutropenia with obvious leukocytosis (> 20 x 109 / L)
- The usual feature is myeloid cells shifted to the left.
- Causes include:
1. Infections
2. Marrow infiltration
3. Systemic disease (AGN & Acute liver failure)
Quantitative changes (NEUTROPENIA)
Neutropenia is reduced the number of circulating neutrophils
- Mild (1- 1.5 x 109/L)
- Moderate (0.5 – 1 x 109/L)
- Severe (<0.5 x 109/L)
• Symptoms are rare with the neutrophil count above 1 x 109/L
• Bacterial infections are the commonest
• Fungal, viral, and parasitic infections are relatively uncommon.
Causes of Neutropenia
- Racial
- Congenital
- Cyclical neutropenia
- Marrow aplasia
- Marrow infiltration
- Megaloblastic anemia
- Acute infections: Typhoid, Military TB, viral hepatitis.
- Drugs
- Irradiation exposure
- Immune disorders: HIV, SLE, Felty’s syndrome, Neonatal isoimmune, and autoimmune neutropenia
- Hypersplenism
Pathologic features
The changes in the bone marrow depend on the underlying mechanism.
- Hypercellular marrow; is seen when the neutropenia results from excessive destruction of the mature neutrophils or from ineffective granulopoieses, such as occurs in megaloblastic anemia.
- Marked decrease in maturing granulocytic precursors in the marrow; associated with the use of agents such as drugs that suppress granulopoiesis.
- All marrow elements are suppressed; seen after treatment with most myelotoxic drugs.
The main problem is infections. They commonly take the form of ulcerating, necrotizing lesions of the mouth, pharynx.
These lesions often show a massive growth of microorganisms.
Lymphopenias are associated with
1. Congenital immunodeficiency diseases
2. Acquired in association with:
- Advanced HIV infection
- Treatment with corticosteroids and other immunosuppressive therapy
- Hodgkin disease
- Widespread irradiation
Management of Neutropenia
- Remove the cause if possible
- Treat any infection aggressively
- Role of Growth factors and Splenectomy
Cyclical neutropenia
- Regular recurring episodes of severe neutropenia (<0.2 x 109/L) usually lasting for 3-6 days
- Can be familial & inherited with maturation arrest
- Three suggested mechanisms for cyclical neutropenia
1. Stem cell defect & altered response to growth factors
2. Defect in humoral or cellular stem cell control
3. Periodic accumulation of an inhibitor
Quantitative changes (EOSINOPHILIA)
- Increase in the eosinophil count must prompt for further investigation (>0.6 x 109/L)
- The causes of eosinophilia can be considered under the following headings
• Allergy: Atopic, drug sensitivity, and pulmonary eosinophilia
• Infection: Parasites, recovery from infections
• Malignancy: Hodgkin’s disease, NHL and myeloproliferative disorders
• Drugs
• Skin disorders
• Gastrointestinal disorders
• Hypereosinophilic syndrome
Hypereosinophilic syndrome
- Criteria of diagnosis:
• Peripheral blood eosinophil >1.5 x 109/L
• Persistence of counts more than 6 months
• End organ damage
• Absence of any obvious cause for eosinophilia
- Most involved Organ: Heart, Lung, Skin, Neurological.
Quantitative changes (MONOCYTOSIS)
- Absolute monocyte count is age-dependent
- Count rarely exceeds >1.0 x 109/L
- Have no marrow reserves
- Useful harbinger of engraftment
- Causes of monocytosis can be grouped as:
• Infection: Chronic infection (tuberculosis, typhoid fever, infective endocarditis), acute infection recovery
• Malignant disease: MDS, AML, HD, NHL
• Connective tissue diseases: Ulcerative colitis, Sarcoidosis, Crohn’s disease
• Post splenectomy
Quantitative changes (BASOPHILIA)
- Basophils are the least common among granulocytes
- Adult reference range for is 0 – 0.2 x 109/L
- Most associated with hypersensitivity reactions to drugs or food
- Inflammatory diseases such as RA and ulcerative colitis are sometimes also associated with basophilia
- Myeloproliferative disorders
- Chronic myeloid leukemia
Quantitative changes (LYMPHOCYTOSIS)
- Blood accounts for only a few percent of lymphocytes throughout the body
- The most compatible variation is seen with age
- Alteration of lymphocyte counts can result from:
• Redistribution of lymphocytes: leading to changes in counts in continuous measurements
• Absolute increase of lymphocyte number
• Loss of lymphocytes
• Combination of these
Non-malignant causes of lymphocytosis
1. Infections:
a. Viral infections: Infectious mononucleosis, CMV, Rubella, hepatitis, adenoviruses, chickenpox, dengue
b. Bacterial infections: Pertussis, Healing TB, typhoid fever
c. Protozoal infections: Toxoplasmosis
2. Allergic drug reactions
3. Hyperthyroidism
4. Splenectomy
5. Serum sickness
Infectious Mononucleosis
a. Epstein-Barr virus
b. Saliva from an infected person is the main contagion
c. The virus infects epithelial cells and B cells
d. Autocrine growth stimulation
e. Infection in children under the age of 10 does not cause illness and result in lifelong immunity
f. Clinical features
1. Fever, malaise, fatigue, sore throat, diagnostic red spots at the junction of the soft and hard palate, splenomegaly
2. Blood picture shows leukocytosis (10 – 20 x 109/L) due to an absolute increase in the number of lymphocytes
3. Diagnosis is by serological tests
4. There is no specific treatment
Quantitative changes (Lymphopenia)
- Lymphocyte count on complete blood count in an adult patient that is below the lower limit of the normal range.
- Lymphopenia is a common finding, especially in elderly patients, which usually has no clinical significance.
It is not recommended to conduct further investigation on elderly patients with lymphocyte count> 0.5 x109/l without any related symptoms.
- Lymphopenia may reflect a response to stress, such as acute infections, recent surgery, or iatrogenic following medications, especially immunosuppressants such as steroids.
Most cases are reversible and do not require expert evaluation.
- Significant lymphopenia:
• Lymphocyte count <1 x 109/l and symptomatic patients (weight loss, fever, drenching night sweats)
• Patients with lymphadenopathy (nodes > 1 cm) and/or splenomegaly.
Causes
Most of the time, lymphopenia is an acquired disease. However, sometimes it may exist from birth.
Some factors that may cause acquired lymphopenia include:
- Fasting or malnutrition
- Severe physical stress
- Cancer treatments (radiation therapy and chemotherapy)
- Use of steroids
- Autoimmune diseases (rheumatoid arthritis, lupus)
- blood disorders (Hodgkin’s disease and aplastic anemia)
- infectious diseases like HIV, tuberculosis, and viral hepatitis
Qualitative changes (MORPHOLOGY)
- Congenital
• Pelger-Huet abnormality: bilobal and occasional unsegmented neutrophils, autosomal recessive genetic disease.
• Hypersegmented neutrophil: autosomal dominant inheritance is rare, and the function of neutrophils is normal.
• May-Hegglin abnormality: Neutrophils contain basophilic inclusions of RNA.
Occasionally there is associated leucopenia. Thrombocytopenia and giant platelet are frequent.
• Alder's abnormality: Granulocytes, monocytes, and lymphocytes contain particles that are dyed purple by Romanowsky dye. Granules contain mucopolysaccharides.
• Chediak-Higashi syndrome: Autosomal recessive disorder. Giant granules in granulocytes, monocytes, and lymphocytes. Partial oculocutaneous albinism.
Depressed migration and degranulation. Recurrent pyogenic infections. Lymphoproliferative syndrome may develop. Treatment is BMT.
- Acquired
• Toxic granulation
• Dohle bodies
• Pelger cells
• Hypersegmented neutrophils
Qualitative changes (FUNCTIONAL)
- Leucocyte adhesion deficiency
- Chronic granulomatous disease
- Chediak-Higashi syndrome
- Primary immunodeficiency
• Severe combined immunodeficiency
• Common variable immunodeficiency
• Isolated IgA deficiency
• T-cell immunodeficiency
• Thymic aplasia (Di George syndrome)










Comments
Post a Comment