Glucose-6-Phosphate Dehydrogenase Deficiency (G6PDD)
- G6PD is a metabolic enzyme required in the pentose phosphate pathway and is particularly important in red blood cell metabolism.
The function of G6PD:
• Regenerates NADPH, allowing regeneration of Glutathione.
• Protects against oxidative stress.
• Deficiency of G6PD leads to hemolysis during oxidative stress- infection, medication, fava beans.
• Oxidative stress causes the formation of Heinz bodies and extravascular hemolysis.
- It is the most common red cell enzyme disease related to hemolysis.
- Large no. of abnormal genes code for the G6PD.
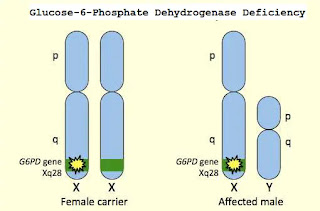
- X-linked disease, lead to G6PD Deficiency (RBCs enzyme deficiency) asymptomatic unless Oxidative stress causes the RBC’s to break apart.
- Inherited –, Recessive.
- The gene of G6PD is present on the X chromosome.
- Therefore, the deficiency state is a sex-linked trait
- Affected males inherit the abnormal gene from their mother, who is usually a carrier (heterozygous).
G6PD variants:
• There are more than 400 variants of G6PD enzyme:
• G6PD A and G6PD B are well-known variants.
G6PD B: The normal G6PD enzyme.
- G6PD A: Found to have normal enzyme activity, but the difference from B is a single amino acid substitution, Lead to different electrophoretic mobility
• G6PD A: the common one associated with hemolysis, electrophoretically identical to A but has only 5- 15% of the normal enzymatic activity.
• Mediterranean G6PD: Same as B in electrophoresis, but its activity is usually 1% lower than normal.
World Health Organization classifies for G6PD genetic variants:
• Class I: Severe deficiency (<10% activity) with chronic (nonspherocytic) hemolytic anemia.
• Class II: Severe deficiency (<10% activity), with intermittent hemolysis.
• Class III: Mild deficiency (10-60% activity), hemolysis with stressors only.
• Class IV: Non-deficient variant, no clinical sequelae.
• Class V: Increased enzyme activity, no clinical sequelae.
What happens in G6PD deficiency?
Cause of G6PD deficiency:
• Individuals who have inherited one of the many G6PD mutations do not show clinical manifestation.
• Some of the patients with G6PD develop hemolytic anemia if they are exposed or ingest any of the followings oxidizing agents:
1-Oxidant drugs:
- Antibiotics: e.g. co-trimoxazole, sulfanilamide, dapsone, Salazopyrin, nitrofurans, chloramphenicol.
- Antimalarials (e.g. primaquine, pamaquine, Fansidar, chloroquine, Maloprim)
- Antipyretics: e.g. aspirin.
- Antihelminths: (e.g. β-naphthol, stibophen.
- Miscellaneous: e.g. vitamin K analogs, naphthalene, probenecid.
2- Favism:
The hemolytic effect of ingesting fava beans is not observed in all individuals with G6PD deficiency but all patients with favism have G6PD deficiency.
Pathophysiology:
• Oxidative denaturation of hemoglobin is the major cause of H.A in G6PD deficiency.
• It is important in the conversion of glucose-6- P to phosphogluconate.
• For subsequent production of NADPH & reduced glutathione (GSH).
• GSH protects enzymes & hemoglobin against oxidation by reducing H2O2 & free radicals.
• H2O2 is generated normally in small amounts during normal red cell metabolism.
• Larger amounts produced when an oxidant drug interacts with oxyhemoglobin.
• Normal red cells have sufficient G6PD activity to maintain adequate GSH levels.
• When deficient, red cells fail to produce sufficient G6PD to detoxify peroxide.
• Hb is then oxidized to Hi, heme is liberated from globin & globin denatures producing Heinz bodies.
• Heinz bodies attach to membrane sulfhydryl groups inducing cell rigidity.
• At this point red cells can no longer traverse the splenic microcirculation.
• Hence lysis occurs.
Symptoms:
- Patients with this condition do not display any signs of the disease until their red blood cells are exposed to certain chemicals in food or medicine, or to stress.
- Symptoms are more common in men and may include:
• Dark urine
• Enlarged spleen
• Fatigue
• Pallor
• Rapid heart rate
• Shortness of breath
• Jaundice
Diagnosis of G6PD Deficiency Hemolytic Anemia:
1-CBC: Bite cells, blister cells, irregular small cells, Heinz bodies, polychromasia.
2-Screening: Qualitative assessment of G6PD enzymatic activity.
3-Confirmatory test: Quantitative measurement of G6PD enzymatic activity.
Because of the higher enzyme level in young red cells, a red cell enzyme assay may give a 'false' normal level in the phase of acute hemolysis with a reticulocyte response.
4-Molecular test: Detection of G6PD gene mutation.
5. Special test: Methemoglobin Reduction Test:
- Sodium nitrite converts Hb (hemoglobin) to Hi (methemoglobin).
- Adding methylene blue should stimulate the pentose phosphate pathway, reducing methemoglobin.
- In G6PD deficiency, methemoglobin persists.
• Normal blood → clear red color
• Deficient blood → brown color
Care of G6PD patients:
• The most important measure is prevention – avoidance of the drugs and foods that cause hemolysis.
• Vaccination against some common pathogens (e.g. hepatitis A and hepatitis B) may prevent infection-induced attacks.
• In the acute phase of hemolysis, blood transfusions might be necessary, or even dialysis in acute renal failure.
• Blood transfusion is an important symptomatic measure, as the transfused red cells are generally not G6PD deficient and will live a normal lifespan in the recipient's circulation.
• Some patients may benefit from splenectomy as this is an important site of red cell destruction.
• Folic acid should be used in any disorder featuring a high red cell turnover.
• Although vitamin E and selenium have antioxidant properties, their use does not decrease the severity of G6PD deficiency.



Comments
Post a Comment