Hemoglobin synthesis & catabolism
Hemoglobin synthesis
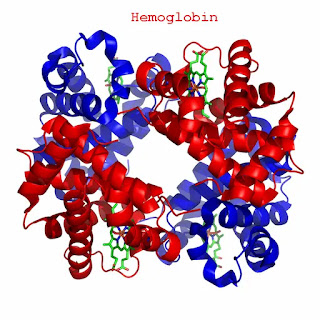
The hemoglobin’s are red globular proteins, which have a molecular weight of about 68,000 and comprise almost one-third of the weight of a red cell.
The hemoglobin is composed of heme and globin.
▪The main function of red cells is to carry O2 to the tissues and to return carbon dioxide (CO2) from tissues to the lungs.
▪To achieve this gaseous exchange the red cells contain the specialized protein hemoglobin.
▪Each red cell contains approximately 640 million Hb molecules.
▪65% of the Hb is synthesized in the erythroblasts, and 35% at the reticulocyte stage.
▪Heme synthesis occurs largely in the mitochondria.
▪Globin synthesis occurs in the polyribosomes.
▪While heme and globin synthesis occur individually inside developing red cell progenitors, their rates of synthesis are orderly coordinated to confirm the optimal efficiency of Hb assembly.
Globin synthesis
▪The various globins that combine with heme to form Hb are all single chain polypeptides.
▪The synthesis of these globins is under genetic control.
▪Humans normally carry eight functional globin chains, arranged in two, duplicated gene clusters: the β-like cluster (β, ϓ, δ, and ε α globin genes) on the short arm of chromosome 11 and the α-like collection (α and ζ globin genes) on the short arm of chromosome 16.
Ontogeny of globin synthesis
Globin synthesis is first noted in the primitive erythroid precursors of the yolk sac at about 3 weeks’ gestation.
▪Embryonic:
Hemoglobin Gower I (ζ2ε2)
Hemoglobin Portland (ζ2ϓ2)
Hemoglobin Gower II (α2ε2)
Fetal: HbF (α2ϓ2), HbA (α2β2)
Adult: HbA, HbA2 (α2δ2), HbF.
Hemoglobin
Each molecule of normal adult hemoglobin (Hb-A) consists of four polypeptide chains α2β2, each with its heme group.
▪Normal adult blood also contains small quantities of two other hemoglobins, Hb-F and Hb-A2. These also contain α chains but with ϓ and δ chains respectively instead of β.
▪The major switch from fetal to adult hemoglobin occurs 3-6 months after birth.
Normal Hb in adult blood
|
|
HbA |
HbA2 |
HbF |
|
structure |
α2β2 |
α2δ2 |
α2ϓ2 |
|
Normal % |
96-98 % |
1.5-3.2 % |
0.5-0.8 % |
Hemoglobin synthesis
▪Heme formation starts with the condensation of glycine and succinyl coenzyme A under the action of a rate-limiting enzyme δ -aminolaevulinic acid synthase.
▪δ-ALA will be formed.
▪Pyridoxal phosphate (Vit. B6) is a coenzyme for this reaction.
▪A series of biochemical reactions will follow.
▪Two molecules of δ -ALA condense to form a pyrrole called porphobilinogen (PBG)
▪Four PBG condense to form a tetrapyrrole uroporphyrinogen III.
▪UPG III is then converted to coproporphyrinogen.
▪CPG then changes to protoporphyrin which ultimately combines with iron in the ferrous state (Fe2+) to form heme.
▪Iron is brought to the developing red cells by a carrier protein (transferrin) which attaches to special binding sites on the surface of these cells.
▪Transferrin releases iron and returns to circulation.
▪Each molecule of heme combines with a globin chain.
▪A tetramer of four globin chains each with its heme group in a pocket is formed to make up a hemoglobin molecule.
▪Heme consists of a protoporphyrin ring with an iron atom at its Centre.
▪The protoporphyrin ring consists of four pyrrole groups that are united by methane bridges (=C-).
▪The hydrogen atoms in the pyrrole groups are replaced by four methylene (CH3-), two vinyl (-C=CH2), and two propionic acids (-CH2-CH2-COOH) groups.
Hemoglobin catabolism (normal red cell destruction)
▪Red cell destruction usually occurs after a mean life span of 120 days.
▪The cells are removed extravascularly by macrophages of the reticuloendothelial system (RES), especially in the bone marrow but also in the liver and spleen.
▪Red cell metabolism slowly decays as enzymes are degraded and not replaced until the cells become non-viable, but the exact reason why the red cells die is obscure.
▪The breakdown of red cells liberates:
1- Iron for recirculation through plasma transferrin to marrow erythroblasts.
2- Protoporphyrin which is broken down to bilirubin.
3- Globins which are converted to amino acids.
Normal red cell destruction
- The bilirubin circulates to the liver where it is conjugated to glucuronides which are excreted into the gut via bile and converted to stercobilinogen and stercobilin(excreted in feces).
- Stercobilinogen and stercobilin are partially reabsorbed and excreted in urine as urobilinogen and urobilin.
▪A small fraction of protoporphyrin is converted to carbon monoxide (CO) and excreted via the lungs.
▪Globin chains are broken down into amino acids which are reutilized for general protein synthesis in the body.
Hemoglobin abnormalities
There are chiefly two types of abnormalities, these are:
▪Quantitative abnormalities: where there is a reduction in the production of certain types of globins e.g.
α thalassemia
β thalassemia
▪Qualitative abnormalities: where there is a production of abnormal hemoglobin e.g. sickle cell anemia.



Comments
Post a Comment