Case Study (6)- Megaloblastic anemia
History:
A 63-year-old woman checked by her general practitioner (GP) complaining of extreme tiredness.She has been increasingly fatigued over the past year but in recent weeks she has become breathless on exertion and complained of headaches.
Her feet have become numb and she has started to become unsteady on her feet.
She has had no significant previous medical illnesses. She is a retired teacher and lives alone. Until the last 2 years, she was active, walking 3 or 4 miles a day.
No history of smoking. She drinks about 15 units of alcohol per week.
She has had no significant previous medical illnesses. She is a retired teacher and lives alone. Until the last 2 years, she was active, walking 3 or 4 miles a day.
No history of smoking. She drinks about 15 units of alcohol per week.
She is taking no regular medication. Her mother and one of her two sisters have thyroid problems.
Her temperature is 37.8°C.
Her pulse rate is 96/min regular, and her blood pressure 142/72 mmHg.
Examination of her cardiovascular, respiratory, and abdominal systems is normal.
She has a symmetrical distal weakness affecting her arms and legs.
Examination:
Her conjunctivae are pale and sclerae are yellow.Her temperature is 37.8°C.
Her pulse rate is 96/min regular, and her blood pressure 142/72 mmHg.
Examination of her cardiovascular, respiratory, and abdominal systems is normal.
She has a symmetrical distal weakness affecting her arms and legs.
Knee and ankle jerks are absent, and she has extensor plantar responses.
She has a sensory loss in a glove and stocking distribution with a particularly severe loss of joint position sense.
MCV: 112 fL (80–99 fL)
WBC: 3.3 X 109/L (3.5–11.0 X 109/L)
PLT: 102 X 109/L (150–440 X 109/L)
Sodium: 136 mmol/L (135–145 mmol/L)
Potassium: 4.4 mmol/L (3.5–5.0 mmol/L)
Urea: 5.2 mmol/L (2.5–6.7 mmol/L)
Creatinine: 92 μmol/L (70–120 μmol/L)
Glucose: 4.4 mmol/L (4.0–6.0 mmol/L)
Bilirubin: 45 mmol/L (3–17 mmol/L)
Alanine Transaminase: 33 IU/L (5–35 IU/L)
Alkaline Phosphatase: 263 IU/L (30–300 IU/L)
• How would you investigate and manage this patient?
- There is a family history of thyroid disease. This can cause macrocytic anemia but not to this degree, and hypothyroidism would not explain the other features.
- As in this patient, profound vitamin B12 deficiency also causes peripheral neuropathy and subacute degeneration of the posterior columns and pyramidal tracts in the spinal cord.
- Antibodies to intrinsic factor and parietal cells should be assayed.
- A radioactive B12 absorption test (Schilling test) distinguishes gastric from intestinal causes of deficiency.
Investigations:
CBC:
HGB: 4.2 g/dL (11.7–15.7 g/dL)MCV: 112 fL (80–99 fL)
WBC: 3.3 X 109/L (3.5–11.0 X 109/L)
PLT: 102 X 109/L (150–440 X 109/L)
Sodium: 136 mmol/L (135–145 mmol/L)
Potassium: 4.4 mmol/L (3.5–5.0 mmol/L)
Urea: 5.2 mmol/L (2.5–6.7 mmol/L)
Creatinine: 92 μmol/L (70–120 μmol/L)
Glucose: 4.4 mmol/L (4.0–6.0 mmol/L)
Bilirubin: 45 mmol/L (3–17 mmol/L)
Alanine Transaminase: 33 IU/L (5–35 IU/L)
Alkaline Phosphatase: 263 IU/L (30–300 IU/L)
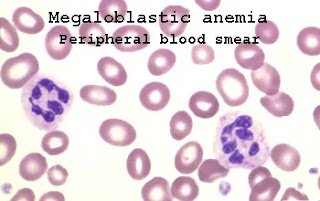
Peripheral blood smear
Questions
• What is the diagnosis?• How would you investigate and manage this patient?
Answers:
• This patient has severe macrocytic anemia and neurological signs due to vitamin B12 deficiency.- There is a family history of thyroid disease. This can cause macrocytic anemia but not to this degree, and hypothyroidism would not explain the other features.
- As in this patient, profound vitamin B12 deficiency also causes peripheral neuropathy and subacute degeneration of the posterior columns and pyramidal tracts in the spinal cord.
Further Laboratory Studies
- Serum vitamin B12 and folate levels should be measured.- Antibodies to intrinsic factor and parietal cells should be assayed.
- A radioactive B12 absorption test (Schilling test) distinguishes gastric from intestinal causes of deficiency.


Comments
Post a Comment